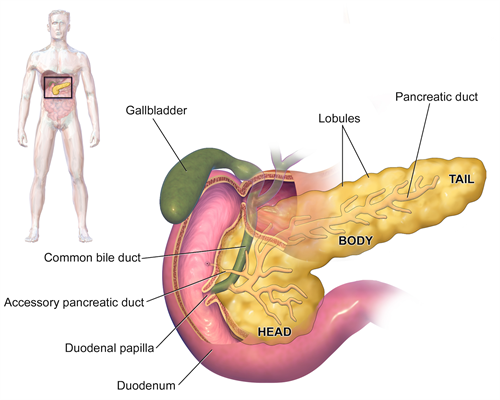
Pancreatic Pseudocysts
A pancreatic pseudocyst is a fluid-filled sac that forms in the abdomen comprised of pancreatic enzymes, blood, and necrotic (dead) tissue. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses and typically are complications of chronic pancreatitis. The prefix pseudo- (Greek for "false") distinguishes them from true cysts.
By BruceBlaus (Own work) [CC BY-SA 4.0], via Wikimedia Commons
Causes
Pancreatic pseudocysts are most often caused by chronic pancreatitis, an inflammation of the pancreas. Other less frequent causes are gallbladder disease, toxicity from medicines, traumatic injury, surgical complications, and congenital conditions.
Symptoms
Symptoms typically include one or more of the following:
- Abdominal tenderness and/or pain
- Diarrhea
- Fever
- Fluid buildup in the abdomen
- Nausea and vomiting
- Tender
- Weight loss
- Yellowish skin and eyes (jaundice)
In some cases, pseudocysts have no symptoms.
Diagnosis
Cyst Fluid Analysis
- Carcinoembryonic antigen (CEA) and CEA-125 (low in pseudocysts and elevated in tumors);
- Fluid viscosity (low in pseudocysts and elevated in tumors);
- Amylase (usually high in pseudocysts and low in tumors)
Imaging
- Computerized tomography (CT Scan) for initial assessment and follow-up
- Ultrasonography - The role of ultrasonography in imaging the pancreas is limited by the fact that the pancreas lies behind the stomach (and so a gas-filled stomach will obscure the pancreas).
- Magnetic resonance cholangiopancreatography (MRCP) - to establish the relationship of the pseudocyst to the pancreatic ducts, though not routinely used
Treatment
A small pseudocyst that is not growing or causing symptoms may be watched and managed conservatively. Overall, treatment should be aimed avoiding complications including infection, hemorrhage, and rupture.
Larger cysts have a higher likelihood to become symptomatic and may even require surgery.
Non-Surgical Treatment
-
Monitoring the pseudocyst to determine if it is growing
-
Endoscopic drainage of the pseudocyst - This removes fluid or infection from the pseudocyst. A long, flexible lighted tube called an endoscope is inserted into the mouth and throat and then maneuvered through the esophagus, stomach, and duodenum and into the pancreas. These organs can be visualized on a video screen which is connected to a tiny camera in the tube. Surgical tools positioned on the tube can then drain the fluid.
-
External drainage - This may be necessary if the pseudocyst is infected. A catheter (tube) is placed through the skin to drain the cyst using CT-guided imaging.
Surgery
If the pseudocyst continues to grow and causes pain, surgery may be needed to drain it. The goal of the surgery is to create a connection between the cyst and a nearby organ such as the stomach or small intestine. The pseudocyst is then drained through that organ. Surgical procedures include:
Cystogastrostomy
In this procedure, a connection is created between the back wall of the stomach and the cyst such that the cyst drains into the stomach.
Cystjejunostomy
In this procedure a connection is created between the cyst and the small intestine so that the cyst fluid is drained directly into the small intestine.
Cystduodenostomy
In this procedure a connection is created between the duodenum (the first part of the intestine) and the cyst to allow drainage of the cyst content into duodenum. The type of surgical procedure depends on the location of the cyst. For pseudocysts that occur in the head of the pancreas, a cystduodenostomy is usually performed.
Complications
Complication of pancreatic pseudocyst include:
- Infection
- Hemorrhage - Dangerous blood loss if the pseudocyst injures nearby blood vessels
- Obstruction - Blocked intestines or bile duct
- Rupture - Pseudocyst bursts of ruptures