Pancreatic Cysts
Pancreatic cysts are fluid-filled sacs or growths that develop in the pancreas.
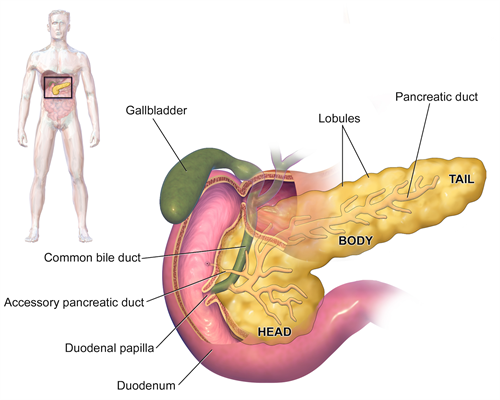
The pancreas is a gland about 6 inches long that is shaped like a thin pear lying on its side between the stomach and the spine. The wider end of the pancreas is called the head, the middle section the body, and the narrow end the tail. The pancreas makes digestive enzymes — juices that help break down food for digestion while endocrine (islet) cells in the pancreas produce hormones, such as insulin, that control blood sugar levels in the body.
By BruceBlaus (Own work) [CC BY-SA 4.0], via Wikimedia Commons
Causes
Some pancreatic cysts occur as a consequence of having pancreatitis, an inflammation of the pancreas. Most, however, develop sporadically without a clear etiology, and are discovered as an incidental finding during a CT or MRI scan done for another purpose. Advances in the field of imaging technology such as 64 and 256-slice CT scanners have dramatically increased the number of pancreatic cysts found as incidental findings.
Most pancreatic cysts are benign (noncancerous) and do not cause symptoms. However, some are precancerous with the potential to develop into pancreatic cancer. It is therefore critically important to identify the type of cyst and whether it has malignant potential.
Types of Pancreatic Cysts
There are approximately twenty types of pancreatic cysts. Among the most common are:
Intraductal Papillary Mucinous Neoplasms (IPMNs)
Intraductal papillary mucinous neoplasms are the most common type of precancerous cyst. These start in the pancreatic ducts, those that connect the pancreas to the intestine. IPMNs produce proteins in large amounts that form mucus or mucin within the cyst lining and fluid. it is difficulty to predict when an IPMN will become malignant (cancerous). IPMNs that involve the main pancreatic duct seem to create a greater risk.
Serous Cystadenomas (SCAs)
Serous cystadenomas are characterized by thick, fibrous walls and are composed of clear fluid. Almost all SCAs are benign. However, they may cause pain, jaundice, and other discomfort as they increase in size.
Mucinous Cystic Neoplasms (MCNs)
Mucinous cystic neoplasms are precancerous growths which start in the body and tail of the pancreas, and develop predominantly in women. Larger cysts with septations, tiny walls that divide the cyst into compartments, may be more likely to become malignant.
Pseudocysts
Pseudocysts are noncancerous (benign) pockets of fluids lined with scar or inflammatory tissue. Because they do not contain the type of cells found in true cysts, they are called pseudocysts. They are a common complication of acute pancreatitis, inflammation of the pancreas. Pseudocysts are unlikely to develop in the absence of pancreatitis or pancreas injury.
Monitoring Pancreatic Cysts
The UCSF Pancreas Center is a high volume center of excellence. Each year, specialists in the program evaluate a wide spectrum of pancreatic cysts, from the most common to rare variants and subtypes, for their malignant potential. The Center also has state-of-the-art monitoring program and conducts research to better identify which cysts are the most dangerous and how best to monitor and treat them.
Diagnosis
Pancreatic pseudocysts may be difficult to diagnose because their symptoms may are similar to other other diseases and condition. Because the pancreas is located deep within the abdominal cavity, cross-sectional imaging is frequently used to locate and diagnose pancreatic cysts and pseudocysts.
One or more of the following tests may be performed to help characterize the type of cyst involved:
- Transabdominal Ultrasound - Sound waves are used to detect a pancreatic pseudocyst, or gallstones that could potentially cause them.
- Abdominal CT (Computed Tomography) scan, which provides more detailed information about the surrounding anatomy and pathology than ultrasound.
- MRI (Magnetic Resonance Imaging) and MRCP (Magnetic Resonance Cholangiopancreatography) which provide a more precise imaging of fluids and debris in pseudocysts than do CT scans.
- EUS (Endoscopic Ultrasound) and Biopsy - In this procedure, a thin needle is inserted into an endoscope.Then ultrasound images are used to guide the needle into the cyst so fluid and cells can be removed. The Carcinoembryonic Antigen (CEA) Blood Test can be done simultaneously to identify the presence of a pancreatic cyst. A pathologist will then analyze this tissue under a microscope to see determine which type of cyst or pseudocyst is present.
- ERCP (Endoscopic Retrograde Cholangiopancreatography) enables a full and detailed visualization of the structure of the common bile duct, other bile ducts, and the pancreatic duct.
UCSF pathologists are experts in analyzing the fluid in pancreatic cysts and determining whether it represents a likely benign course and has malignant potential.
Treatment Overview
Pancreatic cysts with any potential for malignancy must be monitored carefully over time. The decision whether to remove the cyst surgically versus maintaining active surveillance is dependent on the risk or likelihood that the cyst is cancerous or could progress to malignant state at any given time. Balanced against that risk is the fact that pancreatic surgery is a major physically demanding operation. Because of the location of the organ, cysts in the pancreas cannot simply be drained or suctioned out (aspirated).
Surgery to remove some forms of pancreatic cysts may be indicated in the following circumstances:
- The cyst is larger than 3 cm
- The cyst has a solid component
- The main drainage system of the pancreas, the pancreatic duct, has widened or dilated.
- The cyst is growing and is causing pressure or pain on the bile duct of other structures or organs.
Surgery for Pancreatic Cysts
Our surgeons offer a number of options to remove pancreatic cysts dependent on their size and location. Patients may be offered open, laparoscopic, or robot-assisted surgery depending on a number of factors.
The goals of surgery include removal the malignant or pre-malignant lesion and preservation of digestive function.
Studies show that surgical outcomes for removal of pancreatic cysts are best at centers of excellence where cancer surgeons, also known as surgical oncologists, perform a high volume of pancreatic surgeries, and are complemented by a multidisciplinary team of specialists. UCSF pancreatic cancer surgeons are among the most experienced in the U.S. in diagnosing and treating pancreatic cysts.
Open Surgical Procedures
Whipple Procedure
 The Whipple Procedure (also known as a pancreatoduodenectomy) is used to remove cysts in the head of the pancreas. Surgeons remove the head of the pancreas; the duodenum, part of the small intestine; the lower half of the bile duct; the surrounding lymph nodes; the gallbladder, and, in some cases, the pylorus, part of the stomach. (Where the pylorus is not removed, the procedure is called a pylorus-preserving Whipple procedure.) The stomach, bile duct, and remaining part of the pancreas are joined to the small intestine to enable the digestion of food.
The Whipple Procedure (also known as a pancreatoduodenectomy) is used to remove cysts in the head of the pancreas. Surgeons remove the head of the pancreas; the duodenum, part of the small intestine; the lower half of the bile duct; the surrounding lymph nodes; the gallbladder, and, in some cases, the pylorus, part of the stomach. (Where the pylorus is not removed, the procedure is called a pylorus-preserving Whipple procedure.) The stomach, bile duct, and remaining part of the pancreas are joined to the small intestine to enable the digestion of food.
Distal Pancreatectomy
When the cyst is located in the tail or left part of the pancreas, surgeons may perform a distal pancreatectomy, removing the tail of the pancreas, and in most cases the spleen (splenectomy).
Total Pancreatectomy
A total pancreatectomy, complete removal of the pancreas, is recommended when the cyst has involvement throughout the organ. Patients will then need to take insulin and pancreatic enzymes for the duration of their lives.
Minimally Invasive Surgery
UCSF pancreatic surgeons utilize state-of-the-art minimally invasive surgical approaches to treating pancreatic cysts resulting in a smaller incision, shorter hospital stay, faster return to work and daily activities and reduced complications.
Laparoscopy
The surgeon inserts a thin, lighted tube with a video camera at its tip (a laparoscope) through a tiny incision in the abdominal wall, through which the surgeon operates with special instruments.





